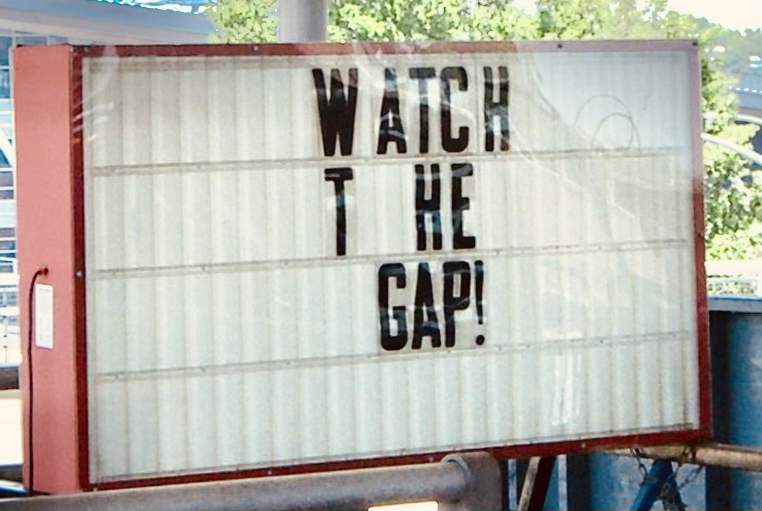
Mind the gap: the importance of a regular independent Gap Analysis
The manufacturers of medical products need to generate evidence to address the requirements and needs of different stakeholder groups. For example, clinical science and regulatory affairs teams optimize development programs to perform clinical trials: aligning on the hypothesis; proper patient selection; the right comparators; primary and secondary endpoints; appropriate duration of the clinical study in order to observe meaningful outcomes; and proper biostatical sample numbers that corroborate the hypothesis. Value and access teams on the other way, are concerned with the clinical, economic, and humanistic evidence needed for submission to Health Technology Assessment (HTA) authorities, payers, hospitals, and health systems, in order to determine the added benefit of a new medical product over the current Standard-Of-Care (SOC). Medical affairs teams generate evidence for specific populations and medical uses derived from registries or investigator-derived studies, and patient experiences under Real-World conditions – which, lead to updated treatment guidelines addressing any gaps from the perspective of key patrons in different countries. And finally, commercial teams try to understand what drives a competitive advantage in the market and the uptake of the new medical product - ensuring appropriate on-label use and the desired financial return.
Clinical evidence can be generated from a range of methods and data sources, such as prospective randomized clinical trials, single-arm trials, real-world data analysis, observational research, and modelling/simulation studies. All of these approaches provide complementary insights, but differ in respect to investment levels, timelines, and validity. All of the data generated requires a detailed assessment of the extent to which it supports the company’s and stakeholders’ expectations regarding the benefit-risk trade-off, and the effectiveness and safety of the new medical product relative to the current State-of-The-Art (SOTA).
As such, it is important to identify any clinical evidence gaps, and prepare risk evaluation and mitigation strategies on a regular basis. The goal is to maintain a running tally of the existing and newly arising evidence gaps; and define clear plans to mitigate them. Conducting this yearly review allows everyone in the organisation - from global functions to country leaders, to have a common view of the clinical evidence needs and a continuous plan for uninterrupted product certification.
Performing Gap Analysis and formulating gap-mitigation strategies is a specialised task that greatly benefits from the involvement of an expert independent professional - one that uses an un-silo outside-of-the-box systematic approach to evaluate the clinical evidence available and what is still missing for a steady continuous product (re)certification.
As such, don’t forget to assess and mitigate any evidence gaps on a yearly regular basis, so your product doesn’t end up falling through the gap.
by Catarina Carrão
(aka Ana Catarina Ribeiro Carrão)